We finance 100% of your treatment plan. We accept all payment types.

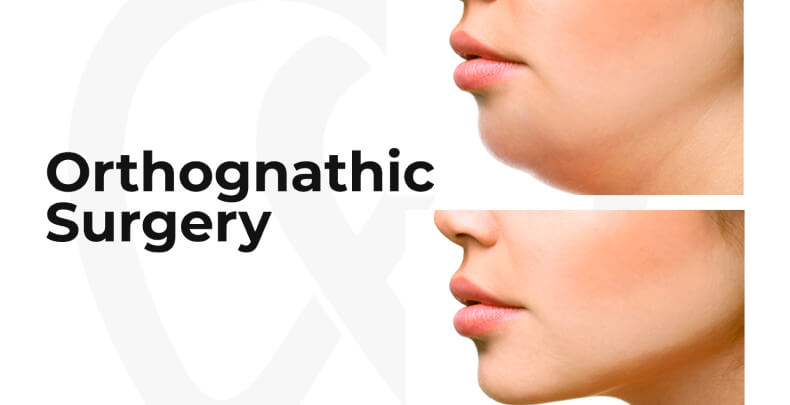
Maxillofacial surgery diagnoses, treats, and surgically rehabilitates alterations of the entire facial structure, whether due to congenital or acquired conditions in the whole Bucco-Dento and maxillary environment.


Bulevar Lázaro Cárdenas 18102 Otay
Constituyentes, 22457, Tijuana, B.C.

First-time patient:
local MX (664) 905-7510
U.S. 619-330-0492
Existing patient:
local MX (664) 905-7503
U.S. 619-734-2331

Mon – Fri: 10:30am – 7:30pm
Saturday: 9:00am – 6:00pm
Sunday: Closed

Av. Sonora #3805 Recta
Chapultepec, Tijuana, B.C.

First-time patient:
local MX (664) 686-3597
U.S. 619-330-0492
Existing patient:
local MX (664) 215-6495
U.S. 619-272-8617

Mon – Fri: 10:30am – 7:30pm
Saturday: 9:00am – 6:00pm
Sunday: Closed

Paseo Pedregal #460 Int. 4
Sección Terrazas de Mendoza,
Playas de Tijuana, Tijuana, B.C.

First-time patient:
local MX (664) 976-5911
U.S. 619-330-0492
Existing patient:
local MX (664) 201-5906
U.S. 619-734-2330

Mon – Fri: 10:30am – 7:30pm
Saturday: 9:00am – 6:00pm
Sunday: Closed

Blvd. Cochimíes #16210
Zona Río 3era Etapa, Tijuana B.C.

First-time patient:
local MX (664) 625-0222
U.S. 619-330-0492
Existing patient:
local MX (664) 660-9505

Mon – Fri: 10:30am – 7:30pm
Saturday: 9:00am – 6:00pm
Sunday: Closed
